By: Amy Kathryn (Katie) White, DO
After a breast cancer diagnosis, under certain circumstances, women may be presented with the opportunity to choose between mastectomy (removal of all the breast tissue) and lumpectomy (removal of the cancerous tissue with a margin of normal breast tissue). If lumpectomy is performed, treatment is usually followed by radiation therapy. The combination of lumpectomy plus radiation therapy is commonly referred to as breast-conservation therapy
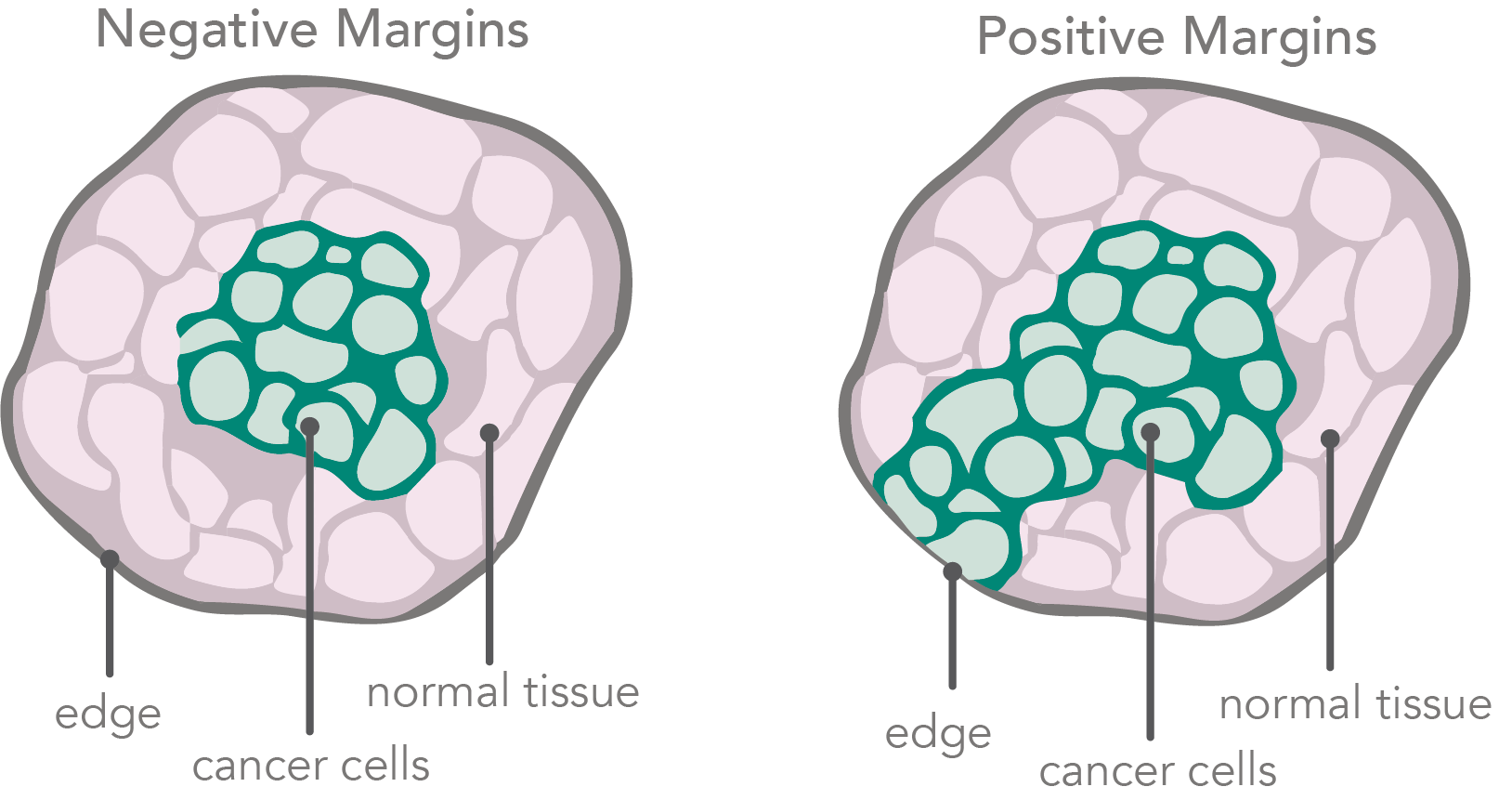
When breast cancer is surgically removed, a rim of normal tissue surrounding the tumor is also removed. This rim is called a margin. Margins help show whether or not all of the tumor was removed. A negative margin means that extra tissue does not contain cancer cells and no additional surgery is needed. A positive margin has cancer cells in the rim of extra tissue. More surgery may be needed to get negative margins.
Over the years, data has shown both to be equally effective in regards to breast cancer prognosis.
Many deciding factors go into the decision of lumpectomy or mastectomy. In general, this is a shared decision between patient preference and breast surgeon recommendations.
The main advantages to lumpectomy include:
- a less invasive surgery
- preservation of appearance and sensation of the breast
- significantly shorter recovery time
The disadvantages include the need for adjuvant (post-operative) radiation therapy which usually lasts 3-6 weeks (depending on your cancer). Radiation therapy in certain patient populations can be deferred; however, is usually recommended to decrease the risk of the cancer coming back locally. There are incidences where someone may not be eligible for breast conservation surgery. You may not be eligible for a lumpectomy if there are multiple areas of cancer in your breast, large breast cancer size, prior radiation to the breast or have contraindications for radiation therapy.
So how did we get here?
In 1882, William Halsted, a surgical innovator and creator of surgical and medical residency training programs, performed his first radical mastectomy for the treatment of breast cancer at Roosevelt Hospital in New York (now part of the Mount Sinai system). Radical mastectomy included the removal of the breast tissue, the underlying pectoralis major and minor muscle, as well as removal of all the lymph nodes under the axilla. He published his data of 50 patients in 1894 which showed excellent clinical results and low local recurrence rates when compared to previous breast cancer treatments previously described. The radical mastectomy became the cornerstone for breast cancer treatment and was universally embraced for all stages of breast cancer. Unfortunately, this surgery resulted in significant chest wall deformity and postsurgical complications such as lymphedema. The use of chemotherapy and radiation had not played a role in breast cancer treatment at that time, so its adjunct use and benefit had not yet been demonstrated.
Around 1956, Bernard Fisher, medical doctor and surgeon, introduced the practice of clinical trials and questioned the need for such radical surgery in all stages of breast cancer. By this time, radiotherapy experiments and usage benefits had been successful in Europe. Fisher used this data and information to create clinical trials to test the hypothesis: “Does less invasive surgery offer the same prognosis in breast cancer treatment?” Over the next 30 years, Bernard Fisher led clinical trials that resulted in transformative changes in the treatment of breast cancer.
The results of multiple clinical trials comparing Halsted’s radical mastectomy to what we know today as a total mastectomy (removal of breast tissue and sentinel node biopsy), as well as comparing to lumpectomy with node biopsy and radiation, showed similar results when comparing overall survival, disease-free survival and local recurrence rate. These three decades of comparison between aggressive radical surgery and less invasive surgery allow breast surgical oncologists to offer the safe and successful option of breast conservation therapy.